This week, the podcast features Part Two of our discussion about ways to expand Medicare to more Americans.
Last week, we spoke with Marilyn Moon, a top expert on Medicare who co-chaired the recent report on expanding Medicare from the National Academy of Social Insurance. That report looked at three different ways to expand Medicare - lowering the eligibility age, establishing Medicare-for-all, and creating a Medicare buy-in.
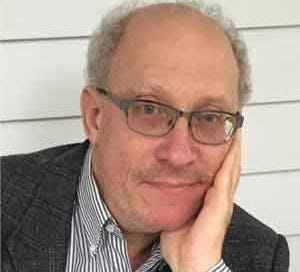
This week, we get a minority report from one of the NASI panel’s dissenting members. Peter Arno is an economist at the University of Massachusetts-Amherst. Peter specializes in social insurance and he’s a strong critic of the for-profit health insurance industry. I spoke this week with Peter to get his perspective on why we need a government-run Medicare for All program as we come out of the coronavirus crisis.
Our conversation was based in part on a recent article on this topic that Peter co-authored, which makes this key point:
There is a large elephant in the room in the national discussion of Medicare for All: the transformation of the US health care system’s core mission from the prevention, diagnosis, and treatment of illness—and the promotion of healing—to an approach dominated by large, publicly traded corporate entities dedicated to growing profitability and share price, that is, the business of medicine.
The problem is not that these corporate entities are doing something they shouldn’t. They are simply doing too much of what they were created to do—generate wealth for their owners. Unlike any other wealthy country, we let them do it. The dilemma of the US health care system is due not to a failure of capitalism or corporatism per se, but a failure to implement a public policy that adequately constrains their excesses.
The problem of employer-based health insurance looms large at a time of mass joblessness, of course. Economist Geoff Sanzenbacher weighs in on this point here, while noting that employer coverate is unequal:
The first reason employer-sponsored health insurance is unequal is because not everyone works. In 2018, about 78 percent of adults age 25 to 64 (the age before Medicare kicks in), were in the labor force. And 2018 was a good economic year. 2020 is not a good economic year. While people who don’t work might be able to get health insurance through a spouse but, as I’ve talked about before, marriage is declining especially for the poor.
Instead, Medicaid sometimes fills the gap for people who are very poor and don’t work. Of course, in some states, this option isn’t available for people without kids. For those who are less poor, the Obamacare Individual Marketplaces might offer an option. Then again, the Trump Administration hasn’t made it a priority to improve those markets. And, the administration hasn’t exactly made enrolling any easier, even for people who have lost their jobs due to the Coronavirus.
OK, but what if we only care about people with jobs? At least these people get insurance. Right? Nope. The figure below shows that health insurance access is much higher for people in high paying jobs. So, the people that can most afford to pay for healthcare even without insurance, are also the most likely to have it. Yikes.

Listen to the podcast interview with Peter Arno by clicking the player icon above; the podcast also can be found on Apple Podcasts, Spotify and Stitcher.
Social Security claiming in the pandemic


Over the past decade, far more workers who are eligible for Social Security have been waiting to file, often substantially increasing their lifetime annual benefits.
But the stunning job losses in the pandemic-induced economic crisis could bring this trend to a crashing halt, as suddenly unemployed older workers without substantial savings scramble to meet living expenses.
In my Retiring column for The New York Times last weekend, I reviewed the pros and cons of different strategies for claiming benefits during the coronavirus pandemic.
Making COVID-19 advance care directive decisions
“I am alarmed that we are not yet thinking ahead.”
So writes Dr. Joanne Lynne in a Health Affairs post, Getting Ahead Of COVID-19 Issues: Dying From Respiratory Failure Out Of The Hospital.
Dr. Lynne, a respected physician on end-of-life care, writes that much more attention needs to be paid to issues such as:
Determining care preferences for people at high risk of dying from COVID-19, so we know whether they want to endure hospitalization and life on a ventilator if they get a bad case;
Getting ready to support peaceful course to death in homes and nursing homes for those who otherwise face suffocation.
There’s much more here if you care to take a deeper dive.
Other articles I’m reading this week
The fight against the coronavirus won’t be over when the U.S. reopens . . . Expert advice on fitness when you’re stuck at home . . . All the places coronavirus lurks (or doesn’t) . . . the Older Americans Act reauthorization was signed into law . . . The late songwriter John Prine always knew loneliness was a public health crisis . . .Medicare Advantage enrollment has grown rapidly over the past decade, and Medicare Advantage plans have taken on a larger role in the Medicare program.
Subscribe now
If you haven’t subscribed to the newsletter, give it a try if your finances permit in this tough economy. You’ll be supporting independent journalism dedicated to covering what matters for older Americans. Subscriptions cost $5 per month or $60 year, and you can cancel at any time.
If not, no worries - I’m committed to providing everything I’ve got on the coronavirus crisis in the free edition for as long as it takes.